There are several methods to assess hearing, each tailored to specific circumstances. The type of test chosen is influenced by factors such as the patient’s age, cognitive abilities, and even the reliability of a patient’s responses. Although most hearing professionals will be able to determine the best type of hearing test for you, it can be helpful to understand the different types of hearing tests to prepare yourself, understand how you will be evaluated for normal hearing or impaired hearing, and more fully recognize the terminology being used by the hearing health professional administering the test. What are the different types of hearing tests?
Comprehensive Audiometry
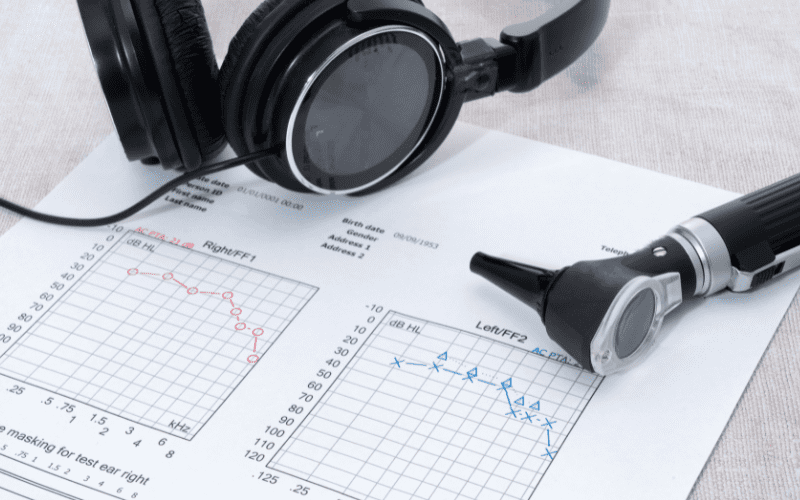
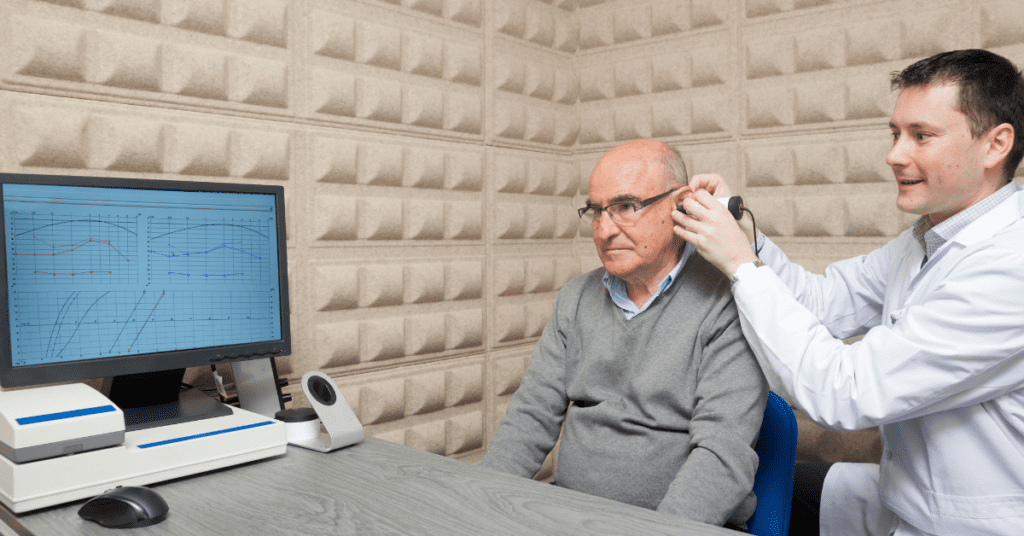
A comprehensive audiometry (or comprehensive audiogram) is the type of test delivered by an audiologist within a clinic setting. This test can be quick depending on the individual, and takes as little as 10-15 minutes in a sound-treated booth. The booth is designed to reduce ambient noise to an acceptable level to meet appropriate standards. Called “comprehensive” for its design to test overall hearing health, an audiogram will be completed at the conclusion of the test, with details involving the success or difficulty in hearing common tones, volumes, and pitches.
Pure Tone Testing
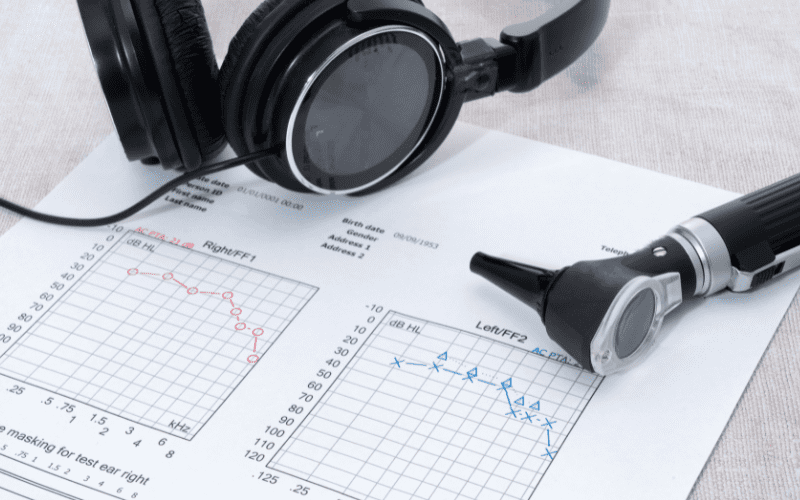
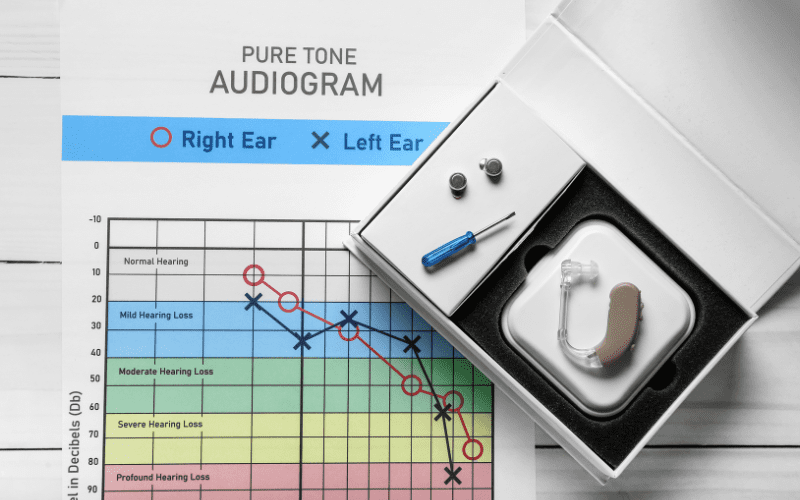
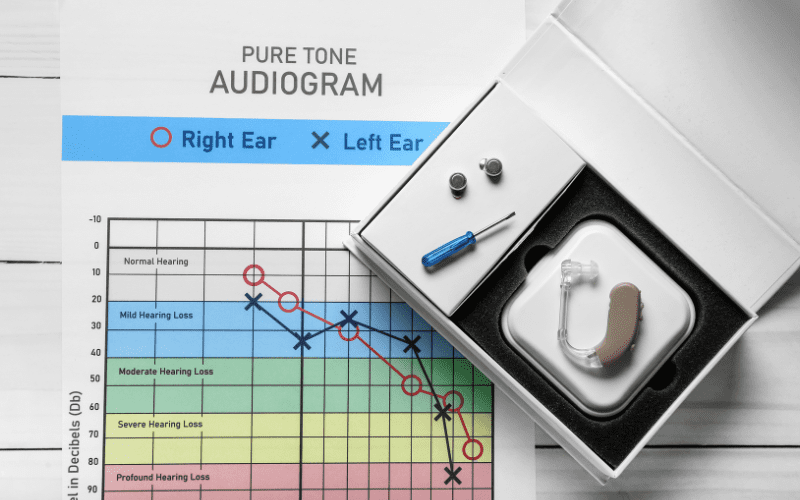
Pure tone testing is often included in a comprehensive audiometry, as it allows audiologists to determine the type, severity, and configuration of an individual’s hearing loss. Different hearing tests measure different aspects of healthy (or unhealthy) hearing, and this one is an important step in determining the degree of an individual’s hearing loss, and can indicate whether the issue is likely to be in the inner, middle or outer ear, based on the responses via air and bone conduction testing. It can help determine if loss is mild or severe hearing loss is present at various frequencies.
"As a recent graduate who’s achieved stage four habituation, I cannot thank Treble Health enough for getting me to the finish line."



"As a recent graduate who’s achieved stage four habituation, I cannot thank Treble Health enough for getting me to the finish line."
– Louis
Book a free consultation to learn which Treble Health solution is right for you. Join Louis and thousands more who have found lasting tinnitus relief.
Pure tones are the “beeps” or soft, clear noises used to evaluate hearing. These tones are tested with either headphones or insert earphones, and a bone oscillator, which is a transducer that sends sounds through vibrations against the mastoid bone of the skull. The responses give us an impression of how well sound is traveling through the outer, middle, and inner ear.
Pure tones’ are measured in terms of intensity and frequency. Within this type of testing, it is important to determine the threshold of the person in question, or the softest level detected at least 50% of the time.The threshold gives information as to how well an individual can hear as compared to normal hearing normative values. It provides information about the patient’s hearing health.

In a pure tone test, the pure tones are delivered through inserts or headphones (called air conduction) and bone oscillators (called bone conduction). In the case of a person who is unable or unwilling to wear traditional headphones, the sound may be transmitted through a speaker system. In all types of hearing tests, patient responses are recorded as the basis of the individual’s hearing health is established.
While the range of human hearing spans from 20-20,000Hz, audiologists and other hearing health professionals typically test within the 250-8,000 Hz range, as it is the range most important for speech sounds. Because communication is one of the most valuable measures of social health, it is often one of the most significant issues reported by patients requesting hearing tests or reporting hearing loss of one kind or another.
Speech Testing
As mentioned above, speech is one of the most valuable measures of social health, so it is crucial to include speech testing as part of a comprehensive exam. There are two types of speech testing: threshold and suprathreshold. The threshold test comes first, as it allows audiologists and other hearing health professionals to determine what level to begin supra-threshold testing, or testing that evaluates at which point listeners are capable of accurately recognizing speech. It also helps to corroborate with the pure-tone thresholds to ensure that the results obtained are accurate. The Speech Reception Threshold (SRT) is the lowest hearing (HL) level at which 50% of two-syllable words are correctly repeated. Hearing thresholds are often cross checked to confirm the reliability of the results and patient’s responses.
During this process, a word recognition score (WRS) is also obtained at a level designed to facilitate the best performance. Patients will be asked to repeat single-syllable words, which are presented at a loud (but comfortable) level. Sometimes testing is completed at normal conversation levels to predict how well an individual is able to hear and understand speech in the real world. Determining the WRS of a patient during testing helps identify the root of pathology, and can even help determine prognostic information to develop effective treatment and rehabilitation. The WRS can also help determine which type of hearing device is most appropriate for the patient.
Different Testing Methods
When a patient is not able to reliably or comfortably participate in voluntary testing, there are modified test techniques that can still effectively measure the health of the outer, middle, and inner ear. These are typically applied to pediatric patients, but there are certainly instances in which an adult patient is not able or willing to respond reliably and the following tests are administered:
- Behavioral Observation Audiometry. This hearing test is used for infants who cannot respond to tones or speech stimuli. Behavior changes, such as the startle response are observed and recorded in response to different sounds. This test is typically given from newborn age to 7 months.
- Visual Reinforcement Audiometry. This test is used for infants and toddlers who can be conditioned to answer reliably. In this test, children are encouraged to respond to a stimulus by pairing that stimulus with an interesting sight like a moving toy or video clip. It is typically used from 7 months to 2.5 years.
- Conditioned Play Audiometry. This test is used for young children, over the age of two (typically 2-5 years), who can be conditioned to respond to stimulus in a more complicated effort than the previous test. Stimulus pairing often utilizes more active engagement, such as rolling a ball down a ramp or completing a puzzle after hearing a sound or a word.
A healthcare professional will identify the best possible type of testing to yield effective results. As such, your battery of tests may differ from those of other people with hearing loss.
Tuning Fork Tests



Tuning fork tests are not as technologically advanced as some of the other methods of testing, but are useful, nonetheless. They are quick and easy, and can be used to estimate the type of hearing loss an individual is experiencing. By striking a tuning fork and placing it on the patient’s head in certain spots, then asking them questions about what they hear, healthcare professionals can arrive at several conclusions regarding the patient’s degree and type of hearing loss.
Although it is useful, there are those who question its reliability; it is not typically used as a standard test, but is instead used when no other information or technology is available. It is not typically used as a diagnostic tool in isolation.
Immittance
Immittance testing measures the status and the function of the middle ear system–in particular, the tympanic membrane and acoustic reflex. Because the vibration of this membrane and contraction system is integral to healthy ear function, an immittance test can help determine if the middle ear is functioning as it is supposed to. Unlike age related hearing loss, loss involving damage to the tympanic membrane may be more likely to be related to injury, infection, or trauma. Immittance testing provides information that can help guide medical treatment, and help either confirm or disprove additional test results.
Tympanometry
Tympanometry, a form of immittance testing, measures the mobility of the eardrum, gauging the air pressure changes that occur within the ear canal. While it does not directly measure hearing ability, it does help lend insight into a variety of other tests; after all, the tympanic membrane is a vital player in hearing ability. When it is not functioning properly, consistent and appropriate hearing cannot take place. It can identify if there is a perforation in the eardrum, fluid behind the eardrum, or negative pressure behind the eardrum.
Acoustic Reflex Testing
The acoustic reflex is a reflex within the human auditory system that occurs when exposure to loud sounds takes place. When a loud noise is heard, the muscles found in the middle ear contract. In this form of immittance testing, this response is measured and results are used to provide information about the integrity of the auditory pathways ascending through the brainstem. When the muscles do not contract, or do not contract fully, hearing health is impaired, and a patient’s hearing health and path forward can more effectively be determined.
Objective Testing
Objective testing is a form of testing that is more frequently used in infants, and those without the ability to effectively communicate. Behavioral testing is the standard in modern hearing test batteries, but there are cases in which these types of hearing tests are not viable. Objective measurements that do not require cooperation can be delivered in order to better deliver hearing tests to infants and those with communication barriers. Even without communication, these measurements can provide a surprising amount of information regarding the health and efficacy of the hearing system, which allows healthcare providers to confidently diagnose and treat hearing loss.
Otoacoustic Emissions
Otoacoustic emissions are responses measured from the sensory organs found within the inner ear, or the hair cells required for healthy hearing. Normal outer hair cell function is essential to be able to reliably hear soft sounds. When hair cells are damaged, reduced or absent responses are measured on an otoacoustic emissions hearing test, and healthcare professionals can more effectively develop a treatment plan.
Auditory Brainstem Response
The auditory brainstem response test determines how well the brain is taking in and interpreting sound. When sound waves enter the ear, there is a series of electrical impulses that can be measured within the brain to provide information about the signals being transmitted through auditory pathways. Within the first 10 milliseconds after stimulating the hearing system, information is gathered that provides invaluable information regarding the auditory pathway’s integrity. It is even able to provide threshold information with enough specificity to fit hearing aids on infants.
Auditory Steady State Response
A final objective measurement test, the auditory steady state response evaluates whether or not the auditory system is responding to incoming stimuli. Responses are measured and interpreted via an algorithm on a computer, to determine whether responses are present or absent. This can help healthcare providers develop an estimated audiogram to successfully create treatment plans.
The Role Of Testing In Treatment



While it may seem straightforward to suggest that hearing difficulty requires a hearing aid, addressing hearing loss involves a variety of approaches and the common disorders that accompany it. Typically, the standard test battery for hearing assessment begins with pure-tone and speech audiometry, followed by immittance testing, which may include acoustic reflex testing depending on individual circumstances. Depending on these results, Otoacoustic Emissions testing may also be performed. Audiologists and other hearing health professionals play a crucial role in selecting these tests and interpreting their outcomes. This determines the appropriate course of action to effectively treat or manage hearing loss. Other specialized tests and methods are usually reserved for children or individuals who are non-compliant with standard testing protocols.
Next Step: Book Free Consultation
- 75% of patients reduced their tinnitus within three months after following our recommendations.
- "I feel like Treble Health literally gave me my life back." - Randy S. (verified customer)
- Join thousands of people who have reduced their tinnitus after scheduling a free consultation.